If Tips Fails Does It Mean Varices Will Form Again
Overview
What are esophageal varices?
Varices are veins that are enlarged or swollen. The esophagus is the tube that connects the throat to the stomach. When enlarged veins occur on the lining of the esophagus, they are called esophageal varices.
Who is at risk for esophageal varices that break open and bleed?
Not everyone who develops esophageal varices will have bleeding. Factors that increase the risk for bleeding include:
- High portal blood pressure: The higher the portal pressure, the greater the risk of bleeding.
- Large varices: Risk of bleeding increases with size of varices.
- Severe liver disease: Advanced cirrhosis or liver failure increases the risk.
- Ongoing alcohol consumption: In patients with varices due to alcohol, continuing to drink increases the risk of bleeding.
Symptoms and Causes
What causes esophageal varices?
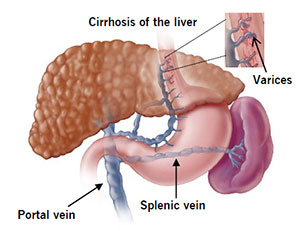
The liver is the organ that cleanses toxins (poisons) from the blood. The portal vein delivers blood to the liver. Esophageal varices usually occur in people who have liver disease. Blood flow through the liver slows in people who have liver disease. When this happens, the pressure in the portal vein goes up.
High blood pressure in the portal vein (portal hypertension) pushes blood into surrounding blood vessels, including vessels in the esophagus. These blood vessels have thin walls and are close to the surface. The extra blood causes them to expand and swell. Varices also can develop in the small blood vessels in the upper part of the stomach.
If the pressure caused by the extra blood gets too high, varices can break open and bleed. Bleeding is an emergency that requires urgent treatment. Uncontrolled bleeding can quickly lead to shock and death.
Thrombosis (blood clot) in the portal vein or the splenic vein, which connects to the portal vein, can cause esophageal varices.
Two rare conditions that can cause esophageal varices are Budd-Chiari syndrome (blockage of certain veins in the liver) and infection with the parasite schistosomiasis.
What liver conditions can lead to esophageal varices?
Any type of serious liver disease can cause esophageal varices. Cirrhosis is the most common type of liver disease. More than 90% of these patients will develop esophageal varices sometime in their lifetime, and about 30% will bleed.
In patients who have cirrhosis, large sections of scar tissue develop throughout the liver and cause blood flow to slow. Cirrhosis can be caused by alcoholic liver disease, fatty liver disease, viral hepatitis or other diseases of the liver.
What are the symptoms of esophageal varices?
Most people do not know they have esophageal varices until the varices start to bleed. When bleeding is sudden and severe, the person vomits large amounts of blood. When bleeding is less severe, the person may swallow the blood, which can cause black, tarry stools. If bleeding is not controlled, the person may develop signs of shock, including pale, clammy skin, irregular breathing and loss of consciousness.
Diagnosis and Tests
How are esophageal varices diagnosed?
Regular screening for esophageal varices is recommended for people who have advanced liver disease. Screening is done by endoscopy. An endoscope is a thin, flexible tube with a light and a tiny camera on the tip. The physician passes the endoscope down the esophagus, and the camera sends images of the inside of the esophagus to a monitor. The physician looks at the images to detect enlarged veins and grades them by size. Red lines on the veins are a sign of bleeding.
The physician may also use the endoscope to examine the stomach and the upper part of the small intestine. This is called an esophogastroduodenoscopy (EGD).
Imaging by CT or MRI scan is also used to diagnose esophageal varices, often in combination with endoscopy. The pictures created by CT or MRI show the esophagus, the liver and the portal and splenic veins. They give the physician more information about the liver's health than endoscopy alone.
Management and Treatment
How are esophageal varices treated?
The goals of treatment are to:
- Prevent more liver damage.
- Prevent varices from bleeding.
- Control bleeding if it occurs.
Preventing liver damage
People who have liver disease need to avoid toxins that cause additional stress on the liver and more damage to it. Some suggestions for maintaining a healthier liver include:
- Avoid alcoholic beverages of any kind.
- Limit use of household cleaners and chemicals.
- Eat a healthier diet that is low in fat and high in fruits and vegetables, whole grains and lean proteins.
- Maintain a healthy body weight (excess body fat puts stress on the liver).
Preventing bleeding
Medications to reduce blood pressure in the portal vein can reduce the risk of bleeding. The most commonly used medications are a group called beta blockers. These include propranolol (Inderal®), nadolol (Corgard®) and carvedilol (Coreg®).
Patients with a high risk of bleeding may undergo preventive treatment with the same techniques that are used to stop bleeding. The most commonly used technique is variceal ligation.
Controlling bleeding
Bleeding from esophageal varices is an emergency that requires immediate treatment. In the hospital, patients receive large amounts of fluid and blood to replace what has been lost.
Two different, non-surgical treatments are available to stop variceal bleeding--variceal ligation performed through an endoscope, and transjugular intrahepatic portosystemic shunt (TIPS) done by a radiologist using x-ray.
- Variceal ligation: In this procedure, tiny elastic bands are wrapped around the varices to cut off blood flow through the varices. This can be performed on as many veins as necessary in one session. After the bleeding is controlled, patients may be given a drug to prevent bleeding from starting again. Variceal ligation should be repeated every 4 weeks until varices have stopped bleeding. An upper endoscopy should be repeated every 6 to 12 months thereafter to make sure no varices have reoccurred. Complications associated with variceal ligation include blood loss, puncture of the esophagus, difficulty swallowing, abnormal heartbeat, infection, fever and reduced or shallow breathing rate. All of these complications are rare.
- Transjugular intrahepatic portal-systemic shunting (TIPS): This is a procedure to reduce portal blood pressure that can be used in patients who have esophageal varices that bleed due to severe cirrhosis. A small, thin tube called a catheter is inserted into a vein in the neck. The catheter is passed through the body to the liver where the hepatic and portal veins are close. (The hepatic vein carries blood from the liver back to the heart.) Next, a wire is passed through the catheter. It is used to poke through the hepatic vein to the portal vein. The wire is removed and a stent (a tiny wire coil) is passed through the catheter to the connection site. The stent is placed in the new channel between the portal and hepatic veins. The stent holds the connection site open so blood can flow more easily from the portal vein to the hepatic vein and exit the liver. This reduces the pressure in the portal vein, which reduces the pressure in the varices, which reduces their risk of bleeding. TIPS can be very effective in preventing bleeding, but it also can cause serious complications, particularly in patients with advanced liver disease, including confusion and liver failure.
Outlook / Prognosis
What is the long-term prognosis (outlook) for people who have bleeding esophageal varices?
Bleeding esophageal varices is life-threatening condition and can be fatal in up to 50% of patients. People who have had an episode of bleeding esophageal varices are at risk for bleeding again.
Treatment with variceal ligation is effective in controlling first-time bleeding episodes in about 90% of patients. However, about half of patients treated with variceal ligation will have another episode of bleeding within 1 to 2 years. Medication and lifestyle changes can help reduce the risk of recurrence (return of bleeding).
Liver transplant many be an option for patients who have severe cirrhosis and/or repeated episodes of bleeding varices. Liver transplant is only performed at selected centers around the country that meet very strict criteria.
greenhalghlaregrell.blogspot.com
Source: https://my.clevelandclinic.org/health/diseases/15429-esophageal-varices
0 Response to "If Tips Fails Does It Mean Varices Will Form Again"
Post a Comment